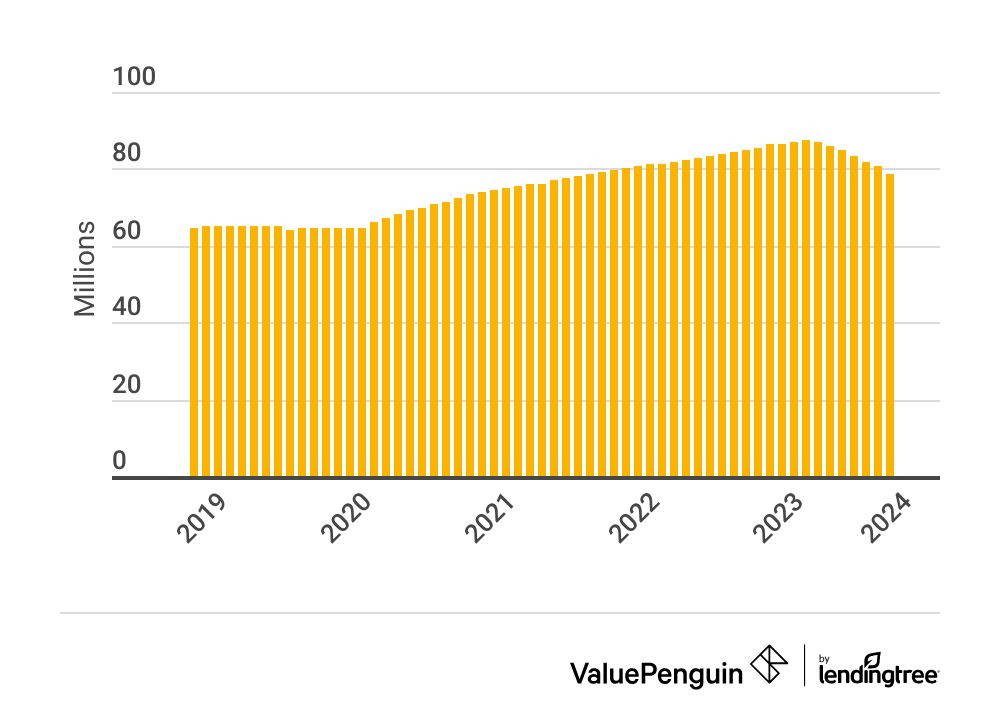
How Has Medicaid Enrollment Changed?
About 86 million people had Medicaid or CHIP at the end of 2023. That's 7% less than 2022.
Find Cheap Health Insurance Quotes in Your Area
How many people are on Medicaid?
There are nearly 79 million people with Medicaid in the U.S.
Since the Medicaid unwinding began in March 2023, Medicaid enrollment has gone down by nearly 9 million people.
On this page
Medicaid enrollment changes
In the past year, Medicare enrollment decreased by 7% nationally.
The largest declines were in Idaho, New Hampshire, Arkansas, Montana, Utah, Texas, Oklahoma, where Medicaid enrollment decreased by more than one-fifth.
Medicaid enrollment by state
State | 2023 | vs. 2022 | vs. 2020 |
|---|---|---|---|
| National | 78,710,401 | -7% | 9% |
| Alabama | 916,217 | -5% | 12% |
| Alaska | 230,760 | -8% | 2% |
| Arizona | 1,917,798 | -10% | 5% |
| Arkansas | 754,560 | -24% | -11% |
| California | 12,577,134 | -1% | 14% |
Total enrollment in November of each year.
Why Medicaid enrollment declined last year
Last year's drop in Medicaid enrollment is largely because of a policy change that forced many people to re-apply for Medicaid. In 2023, a pandemic policy ended that resulted in many people losing coverage. This is called Medicaid unwinding.
How has Medicaid enrollment changed since 2020?
Over the last few years, Medicaid enrollment has increased in some states.
Since 2020, Missouri's Medicaid enrollment has grown by 39%. That's because Missouri expanded its Medicaid program in October 2021, allowing more people to qualify based on their incomes. Medicaid enrollment has also grown by more than 20% in Virginia, Hawaii, Oklahoma, Nebraska, and Oregon.
What is Medicaid?
Medicaid provides free or low-cost insurance for people who have low incomes, disabilities or substance abuse disorders. That's different from Medicare which covers seniors who are older than 65 and those with a disability.
In many states, you're eligible for Medicaid if you're an individual earning less than That's less than $43,056 for a family of four. However, the income limit is lower in states that don't meet the national standards of the Affordable Care Act (ACA).
CHIP health insurance enrollment changes
Enrollment in CHIP (Children’s Health Insurance Program) has grown by 1% between 2022 and 2023.
At a national level, CHIP enrollment has been stable over the past few years compared to the large swings that Medicaid has had.
However, some states have had large changes in CHIP enrollment. Since 2020, CHIP enrollment has fallen by 42% in Texas and has more than doubled in Michigan and Minnesota.
CHIP enrollment by state
State | 2023 | vs. 2022 | vs. 2020 |
|---|---|---|---|
| National | 7,105,426 | 1% | 2% |
| Alabama | 186,108 | -6% | 6% |
| Alaska | 13,433 | 13% | 1% |
| Arizona | 122,286 | -15% | 4% |
| Arkansas | 38,251 | 4% | 5% |
| California | 1,275,670 | -1% | -1% |
Total enrollment in November of each year.
Why CHIP enrollment changes
A rise in CHIP enrollment may be tied to changes in the economy, such as people losing their jobs. It could also be related to many people losing Medicaid coverage. Families who earn too much to qualify for Medicaid may enroll their children in CHIP.
What is CHIP?
CHIP provides health insurance to children in families who earn too much to qualify for Medicaid but earn too little to afford private health insurance. In some states, CHIP also covers those who are pregnant and have a low income.
Where you live and, sometimes, your child's age, determines how much you can make and still qualify for CHIP. Sometimes, you could make more than three times the federal poverty level and still qualify. That's $61,320 per year for a single parent with one child or $93,600 per year for a family of four. However, eligibility varies widely by state.
Medicaid expansion
Medicaid eligibility has been expanded in 41 states — including Washington, D.C.
Most states have chosen to expand who qualifies for Medicaid to meet the guidelines of the Affordable Care Act (ACA). That means Medicaid eligibility is set at 138% of the poverty level, rather than states setting their own rules about who qualifies.

Medicaid expansion states
State | Expanded? | When expanded? |
|---|---|---|
| Alabama | ||
| Alaska | 2015 | |
| Arizona | 2014 | |
| Arkansas | 2014 | |
| California | 2014 |
Income criteria in states with expanded Medicaid
In states that have expanded their Medicaid program, you're eligible for Medicaid if you earn up to $20,783 if you're single or up to $43,056 for a family of four.
That's because you can make 38% more than the federal poverty line and still qualify. The income limit can be even higher if you're pregnant, under 18 or have another special situation.
How to afford health insurance if you earn too much to qualify for Medicaid
If you earn too much to qualify for Medicaid, you can get discounted health insurance by shopping through the marketplace. Depending where you live, that could mean shopping on HealthCare.gov or a website run by your state.
Obamacare subsidies lower the cost of insurance based on your income, and many people who have a low income can get a plan for less than $10 per month.
Medicaid eligibility in states that haven't expanded Medicaid
In states that haven't expanded Medicaid, the income requirements vary widely, and it can be difficult to qualify.
For example, most adults only qualify for Medicaid in Texas with an income less than $4,128 per year. This creates a "coverage gap" where someone can earn too much to qualify for Medicaid and too little to qualify for discounted insurance through the marketplace.
Find Cheap Health Insurance in Your Area
Medicaid unwinding, redetermination and disenrollment
Since the Medicaid unwinding began in March 2023, 60% of all people who have Medicaid have had to reapply for coverage.
That's 49 million people reapplying for Medicaid during the unwinding.
Medicaid unwinding, also called Medicaid redetermination, is the main reason why Medicaid enrollment went down in 2023. The unwinding process meant that those with Medicaid needed to re-apply to keep their coverage, after not needing to re-apply during the pandemic.

- Of the 49 million people in the U.S. who were affected by Medicaid unwinding so far, slightly more than half renewed their Medicaid coverage.
- Medicaid coverage ended for 7% of people who were no longer eligible based on their renewal form.
- Coverage also ended for 18% of people because of administrative reasons such as not reapplying or not having the right paperwork.
Medicaid unwinding results
State | Renewed | Not eligible |
Not re-enrolled
|
|---|---|---|---|
| U.S. | 52% | 7% | 18% |
| OR | 85% | 8% | 5% |
| AZ | 74% | 6% | 14% |
| CT | 74% | 5% | 14% |
| MD | 72% | 8% | 11% |
| NC | 69% | 2% | 14% |
Totals for March through November 2023. Data does not total 100% because pending applications are not shown.
Frequently asked questions
When does Medicaid expansion end?
There isn't an end to Medicaid expansion. Once a state has expanded the income criteria for Medicaid, the new rules stay that way. States can choose to pass a law changing the Medicaid eligibility rules back to before it was expanded. However, no states have done this because it would mean fewer people can afford health insurance coverage.
Did N.C. expand Medicaid?
Yes, North Carolina expanded Medicaid, and more people became eligible for coverage on Dec. 1, 2023. You're now eligible for Medicaid in N.C. if you earn less than $1,676 per month as a single adult or less than $3,450 per month as a family of four. As of March 2024, about 385,000 people have signed up for Medicaid because of the new income eligibility rules.
What is a Medicaid redetermination date?
A Medicaid redetermination date is your deadline to reapply for Medicaid to show that you're still eligible. You'll usually get a letter a month or two before your Medicaid redetermination date telling you that you need to complete a Medicaid renewal form. This form along with any requested paperwork, such as pay stubs or tax returns, needs to be submitted before your redetermination date. If you miss this deadline, you'll lose your Medicaid and will have to reapply, which can take a few months to get coverage again.
Sources
- Medicaid.gov
- Data.Medicaid.gov
- Kaiser Family Foundation
- N.C. Medicaid Expansion Dashboard
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.