Insurance Claim Denials: Worst Companies and How to Appeal
If your claim is denied, your doctor can resubmit the claim, or you can file an appeal to try to get the insurance company to change its decision.
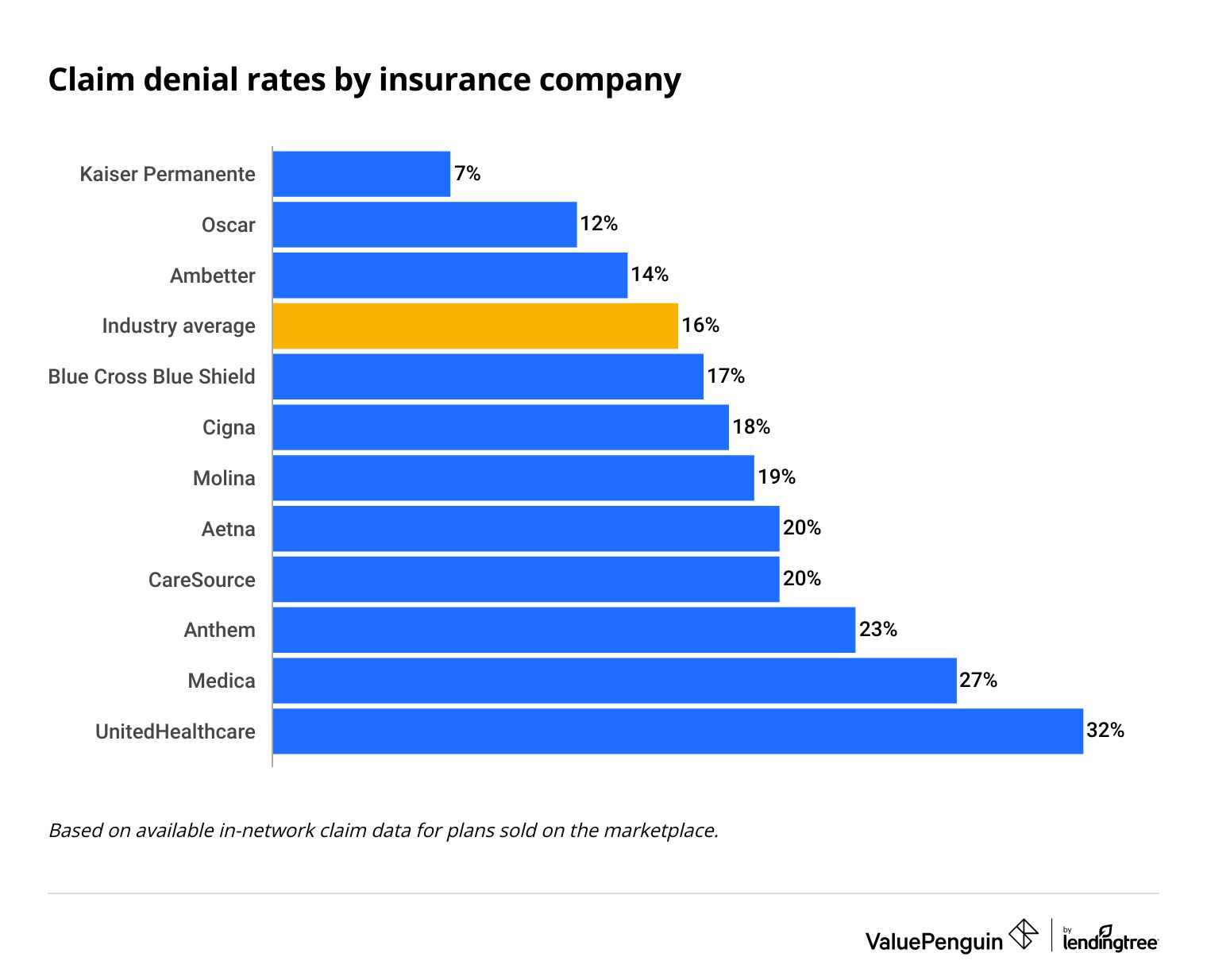
Health insurance claims can be denied because of a simple coding error or because of a more complex problem. The health insurance company you have can affect how likely it is your medical claim will be denied. For example, UnitedHealthcare denies about a third of in-network claims.
Find Cheap Health Insurance in Your Area
Worst insurance companies for paying claims
UnitedHealthcare is the worst insurance company for paying claims with about one-third of claims denied.
Kaiser Permanente is the best large health insurance company for paying claims, denying only 7% of medical bills.
Find Cheap Health Insurance in Your Area
Claim denial rates by insurance company
Company | Claim denials | |
|---|---|---|
| UnitedHealthcare | 32% | |
| Anthem | 23% | |
| Aetna | 20% | |
| CareSource | 20% | |
| Molina | 19% | |
Based on available in-network claim data for plans sold on the marketplace. Anthem is not included in the average for Blue Cross Blue Shield.
What does it mean when insurance denies your claim?
Your insurance claim has been denied when the plan refuses to pay for your medical or prescription costs.
-
The reason why your insurance denied your claim will be in the letter you receive.
The insurance company may say there is a problem with the paperwork or the procedure wasn't a necessary treatment. The reason they denied your claim will be important when deciding what to do next and how you can appeal their decision.
-
Part of a claim may be denied because of one code.
A coding issue could cause insurance to deny all or part of your claim. Depending on which company you have, the claim denial letter may be very clear about what was coded wrong. Or you may have to call them to find out specifically which code is the problem.
-
The insurance company will also send a detailed bill called the Explanation of Benefits (EOB).
This bill will list each individual medical cost, how much has been paid by insurance and how much you owe. Check that the Explanation of Benefits from the insurance company matches the paperwork you received from your doctor or medical provider. For example, both the insurance EOB and an itemized hospital bill should match. Look for coding errors that could have caused your claim to be denied or cost issues, which could affect your total bill.
-
The paperwork may say "patient is not responsible for denied charges."
This means that the claim is not at the stage where they're asking you to pay for the medical procedure. Instead, the insurance company usually needs more information from your doctor's office or medical provider.
-
The letter will also give you information about timing and what happens next.
Typically, when a medical claim is denied because of the paperwork, the insurance company and medical office can work together to sort out the issues. Even if you're not responsible for paying right away, be proactive by calling both the insurance company and medical provider. Once a claim has been denied, you could have one month to resubmit the claim and six months to file an appeal.
Insurance claim denial paperwork may not be straightforward or easy to understand. You may need to talk to the insurance company to fully understand why the claim was denied.
For example, if your surgery bill was denied for not being "medically necessary," there could be a problem with the paperwork, rather than a problem with why your doctor recommended you have the procedure, or they could need documents about your diagnosis.
Top reasons why health insurance companies deny claims
Not getting prior authorization is the top reason why health insurance claims are denied. That's when the insurance company needs to approve the costs of the procedure before you get the medical procedure.

Why insurance doesn't cover hospital bills and medical claims
Reason | Rate |
|---|---|
| No prior authorization from insurance company | 48% |
| Doctor was not covered by plan | 42% |
| Billing code issues | 42% |
| Claim was not submitted before deadline | 35% |
| Patient information was not accurate | 34% |
Based on a survey where medical billing professionals ranked the top three reasons for claim denials
This could help you get your insurance paperwork back quicker after a medical bill. But, it's not yet clear if the high-tech systems are more accurate.
Claim denials because of prior authorization
- Prior authorizations aren't needed in an emergency. If you had an emergency procedure and the claim was denied because you didn't have prior authorization, the insurance company may need you to show paperwork proving that it was an emergency.
- If a claim was denied because an in-network doctor didn't get prior authorization, you usually don't have to pay the bill. When you go to a doctor or hospital that's in your plan's network, the facility is usually responsible for getting prior authorization from your insurance company before doing the procedures. If they didn't get prior authorization, they may be able to work with the insurance company to retroactively get authorization. However, when it's not your fault that the facility didn't get authorization, the doctor's office can't bill you for the procedure if your insurance won't pay.
- If a claim was denied because you didn't get prior authorization for out-of-network care, you could have to pay the full bill yourself. When you go to a doctor or hospital that isn't in your plan's network, you're usually responsible for getting prior approvals for procedures or you can ask your doctor to do it. If you didn't get prior authorization, it doesn't hurt to try to see if the insurance company will change its decision. But you'll typically have to pay for the bill yourself, without the help of insurance.
Claims denied as not being medically necessary
- Claims denied for not being medically necessary may need more paperwork to show that the treatment was needed. This is commonly the issue with straightforward medical claims. For example, if you broke your arm, the insurance company may need the medical records for your broken arm before it will pay for treatment. There could also be an issue where your doctor needs to fix the procedure or diagnosis code for your claim in the paperwork to be covered by insurance.
- When you have complex medical needs, you may need to appeal a claim denial to show that your treatment was medically necessary. In some situations, such as if you have cancer, the treatment that your doctor recommends may not match the insurance company's typical coverage rules. In these cases, talk to both your doctor and insurance company to see what the problem is. If it's not an issue with paperwork or coding, you may need to file an appeal to get the insurance company to give it a more thorough review.
- You probably won't be able to get your insurance to pay for an elective surgery that's not medically necessary. Most insurance plans don't cover surgeries you choose to have, such as LASIK, or cosmetic surgeries such as liposuction. However, check your plan documents because sometimes insurance companies offer discount coupons for some types of elective procedures.
How to dispute your health insurance claim and appeal an insurance denial
Your health insurance plan can't drop you or increase your rates if you appeal a denied claim.
1. Review your plan documents
Start by checking both the letter from the insurance company denying your claim and the plan documents that say what's covered.
- Why the claim was denied
- The list of procedures in the claim
- How much the procedure costs
- How long you have to appeal
- How the appeal process works
- Which procedures are covered
- Coverage rules such as needing prior authorization
- Cost sharing amounts including how much you have to pay before your plan's full benefits begin.
- Which doctors and hospitals are in the plan's network
2. Call your insurance company and doctor to get more info
Call both your insurance company and the billing department of your doctor's office to make sure you understand the claim denial. In a conversation over the phone, it's usually easier to understand what the actual issues are and what can be done to solve it. Many times claims are denied because of simple errors that can be easily fixed.
- Ask your insurance company about why the claim was denied, the company's process for re-reviewing claims, how you can appeal the decision, and what paperwork you need.
- Ask your doctor's office to check the claim, correct any errors, and help you understand why your insurance won't pay.
Tip: Keep detailed records about each phone call and letter. Medical claims can be complex, and sometimes the process is lengthy. Your records can help you keep track of things so you don't miss any deadlines.
3. Have your doctor resubmit the medical bill
Having your doctor's office resubmit a corrected medical claim is usually the first thing you should do after a claim was denied.
Resubmitting the claim is a way to correct any errors with the paperwork or coding. It's also a way to provide additional documentation to the insurance company.
Plans usually have a deadline for resubmitting claims, such as 30 days after it was denied.
Your doctor's office can often be very helpful when you have a claim denied and need to resubmit paperwork. That's because when your claim is denied, the doctor's office has to wait longer to get paid.
4. Request your claim file
An insurance company's claim file will have records of all of the information it considered before denying your claim. Insurance companies are required to send you a claim file within 30 days after you request it.
Your claims file can help you understand the insurance company's decision-making process and what the issues are. This lets you specifically address their problems when you're appealing the claim denial.
For help requesting your claim file:
- Use the ProPublica Claim File Helper which will build a customized letter
- Or use ProPublica's Claim File Request Template if you'd rather fill in the blanks yourself.
5. File an internal appeal
An internal appeal is a way to have the insurance company reconsider a claim that was denied.
-
How long does an appeal take? Internal appeals must be filed within six months of when you found out the claim was denied.
- If you've already had the medical treatment, you'll get a written decision to your appeal within 60 days.
- If you were denied before having the treatment, such as with a prior authorization request, you'll hear back within 30 days.
- In urgent cases, you can make an expedited appeal to get an answer within 72 hours.
-
Can you use an insurance appeal sample letter? Yes, sample appeal letters are a great way to make sure your appeal includes all the information about your claim. There are many good options available online.
- Patient Advocate Foundation's sample appeal letter
- Your state's insurance department also usually has a few templates. For example both North Carolina and Washington insurance departments have templates for common reasons why a claim could be denied.
Your insurance company may also have an appeals form that must be included with your appeal.
Appeal forms by insurance company
Company | Appeals |
|---|---|
| Aetna appeal form | |
| Anthem appeal form | |
| Forms vary by where you live.
Example: Texas Blue Cross Blue Shield appeal form and denial codes list | |
| Cigna appeal form | |
| Humana appeal forms by type of plan |
6. File an external appeal
An external appeal, also called an external review, is a way to get someone outside of your insurance company to review a denied claim.
External reviews are either managed by your state or the Department of Health and Human Services (HHS). To find out which external review process applies to you, check the results of your internal appeal or your Explanation of Benefits (EOB) paperwork that the insurance company sent with your claim denial.
How long does an external review take?
- An external review must be requested within four months after you get results from your internal appeal.
- External reviews must be decided within 45 days after the request is submitted.
- In urgent cases, expedited external reviews must be decided within 72 hours.
Your state's Consumer Assistance Program can help you file external appeals. You can also ask your doctor to file an external appeal for you.
7. Get help with claim denials from other sources
When you're facing a difficult appeals process after a claim denial, use assistance from the government and community groups to help with the process. A range of groups offer that kind of assistance.
- State's insurance department
- State attorney general
- Assistance groups such as SHIP for Medicare
- Consumer Assistance Program (CAP)
- U.S. Department of Labor for appeals about employer plans that are self-funded
As a last resort, you can also contact the media or try to sue the insurance company for denying a claim.
Frequently asked questions
Which insurance company is best at paying claims?
Kaiser Permanente is one of the best health insurance companies for paying claims. It denies only 7% of in-network claims, which is about half of the industry average of 16%.
Can you dispute a medical bill?
Yes, you can dispute a medical bill. Start by calling both your doctor's office and insurance company to understand why your claim was denied or why you were overcharged. You can ask to have the bill resubmitted or file a formal appeal.
Sources and methodology
- Sources include HealthCare.gov and the Centers for Medicare & Medicaid Services (CMS).
- The reasons for claim denials are from Experian's Report of the State of Claims.
- The rate of claim denials by a company are based on available data on claim denials and appeals from CMS public use files. Denial rates look at in-network claims, averaging data for all subsidiaries. Anthem's claims were averaged separately from Blue Cross Blue Shield.
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.







